Inflammatory bowel disease (IBD) is a general term for a group of chronic inflammatory disorders of the intestines characterised by recurrent inflammation in specific parts of the intestines. The primary diseases are Crohn’s disease and ulcerative colitis.
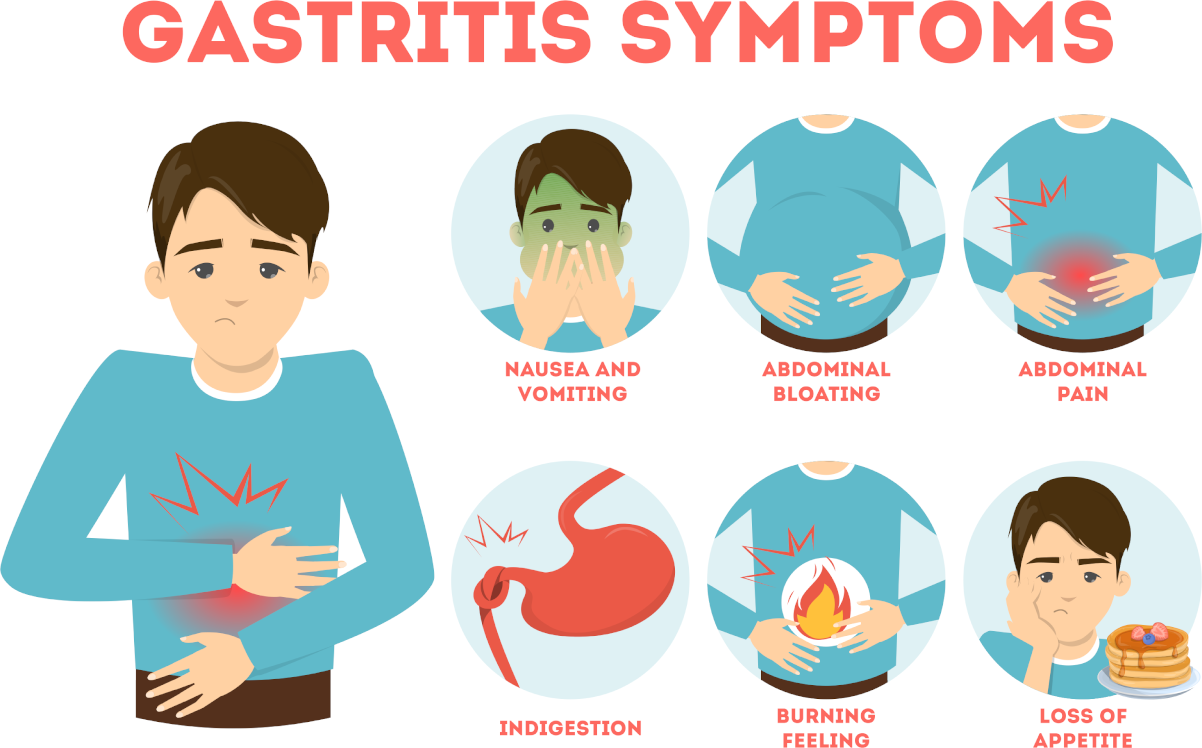
Frequent signs and symptoms
- pain in the left side of the abdomen (the location in the colon) that improves after bowel movements
- attacks of bloody diarrhoea with mucus, alternating with symptom-free periods
- up to 10-20 bowel movements a day
- dehydration
- sweating, nausea
- severe cramps and pain around the rectum
- bloated abdomen
- fever as high as 104°F
- loss of appetite and weight.
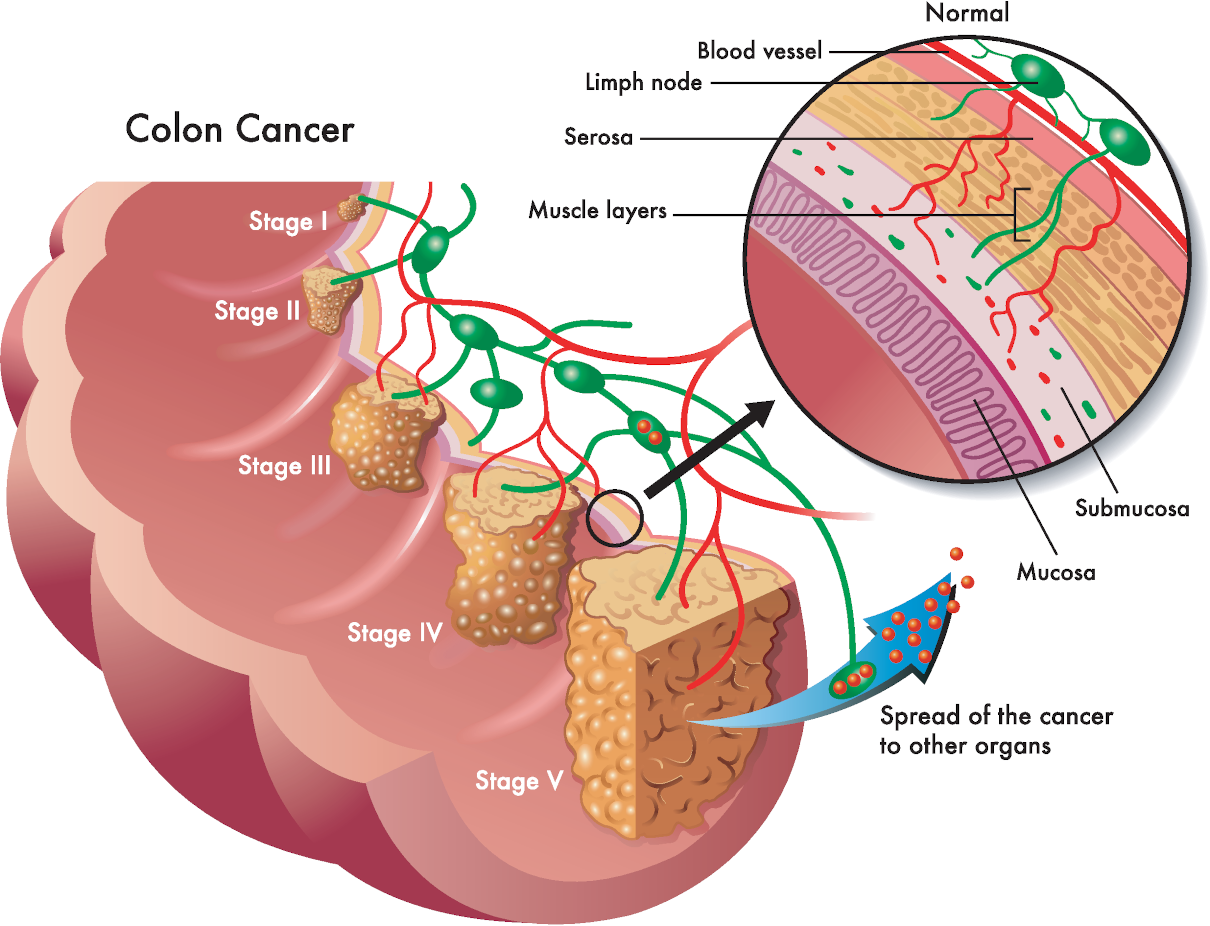
Complications
Complications of Inflammatory bowel disease
- Malnutrition. In 65-75% of IBD sufferers, unhealthy weight loss and undernourishment are prevalent. Contributing factors include decreased food intake (most common cause); diarrhoea-induced nutrient loss (especially electrolytes, minerals and trace minerals); malabsorption in people with extensive small intestine involvement resulting in the decreased absorptive surface as well as bile salt deficiency; overgrowth of unfriendly bacteria in the small intestine; fat malabsorption, which results in significant loss of calories as well as fat-soluble vitamins; protein loss due to increased turnover and shedding of intestinal cells (a substantial loss of blood proteins across the damaged and inflamed intestinal mucosa occurs that may exceed the ability of the liver to replace, even with a high protein intake). Common drugs “the corticosteroids” used in the treatment of Inflammatory bowel disease significantly contribute to malnutrition (corticosteroids stimulate protein breakdown, depress protein synthesis, decrease absorption of calcium and phosphorus, increase urinary excretion of vitamin C, calcium, potassium and zinc, increase levels of blood glucose, triglycerides and cholesterol, increase the requirement for vitamin B6, vitamin C, folate, and vitamin D, decrease bone formation, and impair wound healing)
- Rheumatoid arthritis occurs in about 25% of Inflammatory bowel disease sufferers, consequently affecting the knees, ankles and wrists. Ankylosing spondylitis is infrequent, but symptoms include low back pain and stiffness, eventually limited movement.
- Skin lesions occur in about 15% of sufferers and can be severe but more typically annoying, like mouth ulcers (which appear in 10% of IBD sufferers)
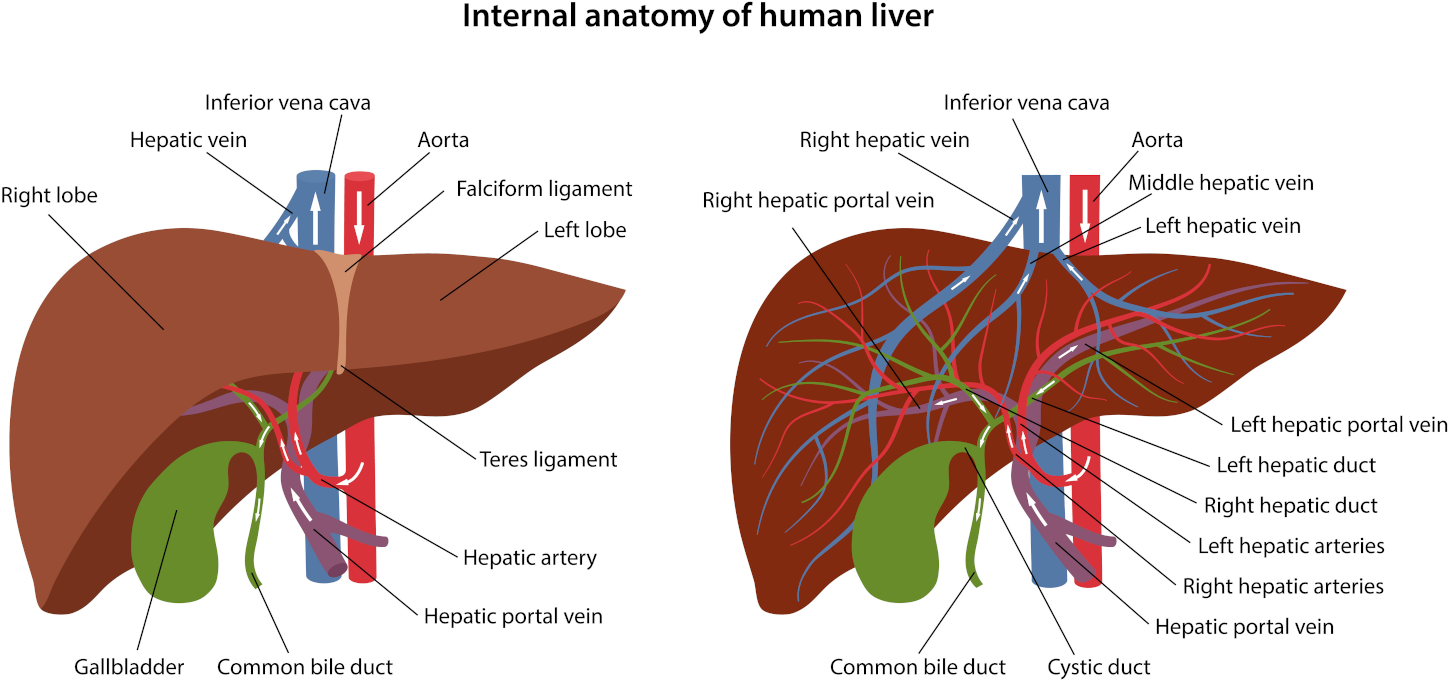
- Severe liver disease affects 1 to 7% of people with IBD and can also be severe. If liver abnormalities are present, then take milk thistle.

Anti-candida Mini Detox – three colonics with bicarbonate of soda
The Anti-candida mini detox involves a concentrated series of three colonics infused with bicarbonate of soda, ideally scheduled once weekly. This regimen serves as a potent initiation into a detoxifying cleansing routine, setting the pace for rejuvenation.
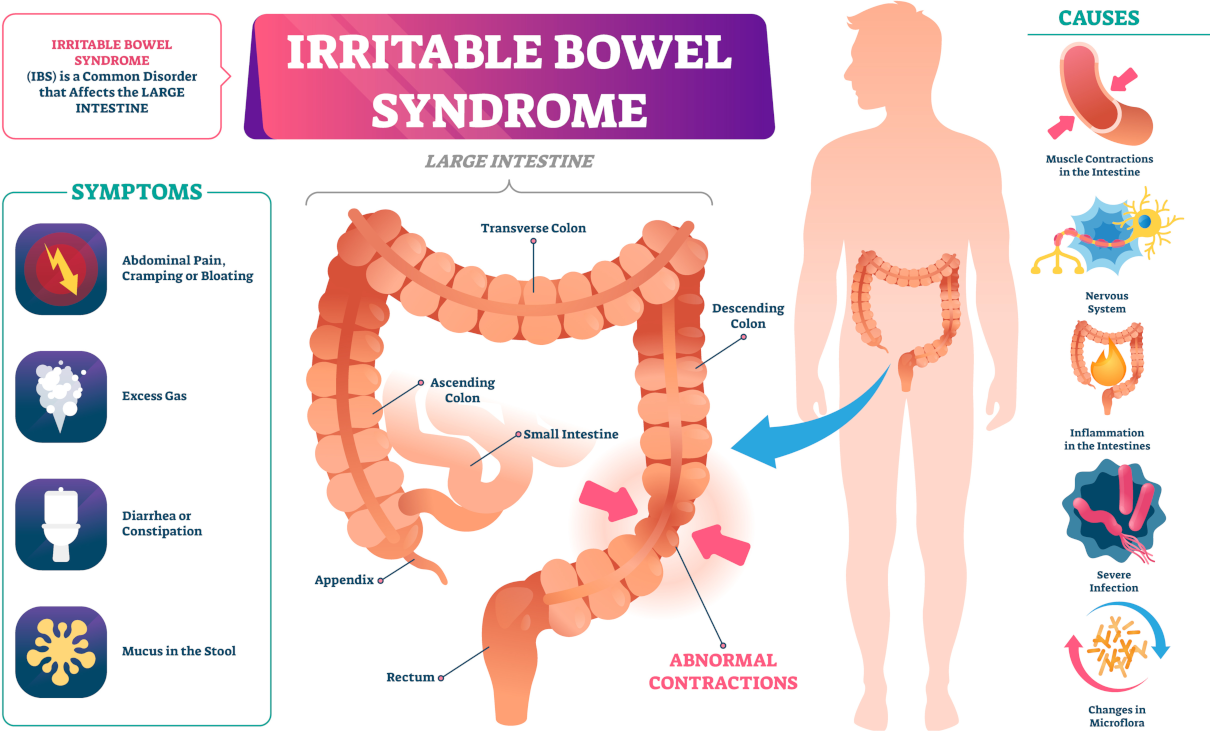
Causes
Causes. No definitive agreement exists as to the origins of IBD. Theories include:
- Genetic predisposition. No specific genetic marker has been found but is likely since IBD is two to four times more common in Caucasians and four times more common in people of Jewish descent. Also, in 15-40% of cases, multiple family members have IBD
- Infections agents. Numerous micro-organisms could also potentially cause IBD. Favoured candidates include mycobacteria and viruses such as rotavirus, Epstein-Barr virus, and cytomegalovirus.
- Antibiotic exposure. Before the 1950s, when penicillin and tetracycline became available in oral form, Crohn’s disease was only found in isolated groups and had a vital genetic component. Since then, the number of cases of Crohn’s disease has risen rapidly in developed countries, especially in the US (and in states that had virtually no reported cases).
- Immune system abnormality. Although immune disturbances are evident in Inflammatory bowel disease, they are most likely a result rather than a cause of the disease process.
- Dietary factors. Several lines of evidence support nutritional factors as the most important causative factor. Crohn’s disease is increasing in countries where people consume a typical Western diet high in saturated fats, refined carbohydrates and sugars. On the contrary, it is almost non-existent where a more ‘primitive’ diet is traditional (high fibre, whole foods). So, food is the dominant factor in determining the intestinal environment. People with ulcerative colitis, however, do not show dietary factors as being a cause compared with controls. In these people, a food allergy may be the most important causative factor
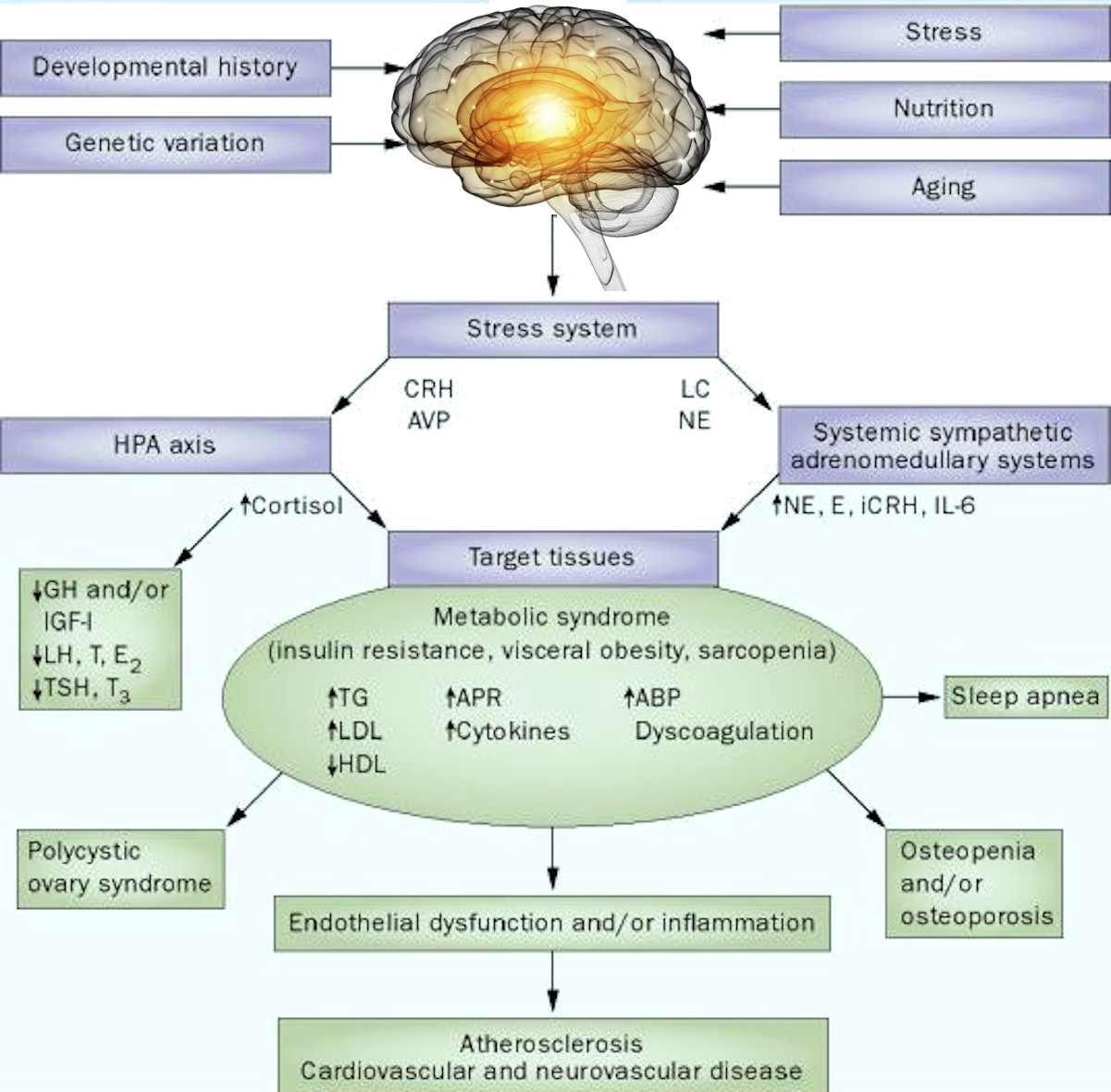
- Emotional factors. While not an initiating condition, psychological factors can significantly affect the course of the disease.
Preventative Measures for Inflammatory bowel disease
- Minimise consumption of sugars and refined foods.
- Eat a health-promoting diet. After identifying and removing any allergenic foods from the menu, choose a balanced diet composed of whole, unprocessed, preferably organic foods, especially plant foods (fruits, vegetables, whole grains, beans, nuts (especially walnuts), and seeds) and coldwater fish such as salmon.
- Take a high-potency multiple vitamin and mineral supplement providing all the known vitamins and minerals and serving as a foundation to build an individualised health-promoting programme.
- Only use antibiotics when necessary.
- Take regular exercise to tone muscles and improve bowel function.
Diet
- Identify and eliminate food allergens
- Eliminate alcohol, caffeine, and sugar as they exacerbate inflammation
- Drink at least two litres of clean water daily to prevent dehydration
- Reduce or eliminate consumption of meat and dairy products while increasing the use of coldwater fish (salmon, mackerel, herring, halibut). Meat and dairy products are the highest sources of arachidonic acid. It is a type of essential fatty acid that the body uses to create inflammatory compounds called leukotrienes, which amplify the inflammatory process and cause intestinal cramping and pain. Coldwater fish are the best source of anti-inflammatory omega-3 essential fatty acids.
- Avoid all foods containing carrageenan. It is a compound extracted from red seaweeds and widely used by the food industry as a stabilising and suspending agent in milk and milk chocolate products (ice cream, cottage cheese, milk chocolate etc.). Researchers have experimentally used carrageenan to induce ulcerative colitis in animals, including primates. In healthy people whose intestines are germ-free, carrageenan does not cause ulcerative colitis. Still, a bacteria found in the faecal cultures of people with ulcerative colitis appears responsible for facilitating carrageenan-induced damage to the intestines.
- People with IBD typically require as much or more than 25% more protein than usual.
- Eat a high-complex carbohydrate, high-fibre diet, which benefits Inflammatory bowel disease. Dietary fibre exerts numerous beneficial effects on the digestive tract, including providing food for health-promoting intestinal flora; soluble fibre slows transit times in individuals with diarrhoea; binds to and removes toxins via faeces. Foods are rich in fibre (legumes, fruits, vegetables) and unrefined carbohydrates (starchy vegetables such as brown rice, barley, millet, quinoa, and spelt). The best additional fibre choices are oat bran and flaxseed meal, which provide soluble fibre. (flaxseed meal also provides omega-3 EFAs).

Food allergy test
Do you experience reactions to foods and think an allergy might cause them? Do you experience hay fever-type symptoms, the cause of which is unknown to you? Allergies can be challenging to pinpoint. And it’s almost impossible to deal with an allergy without identifying what is causing the problem. This Food Allergy Test is a fast and reliable home-to-laboratory allergy testing service.
Supplements
Nutritional supplements
- Flaxseed oil. Take 1 tbsp per day, contains omega-3 EFAs, which the body converts to anti-inflammatory EPA fatty acid.
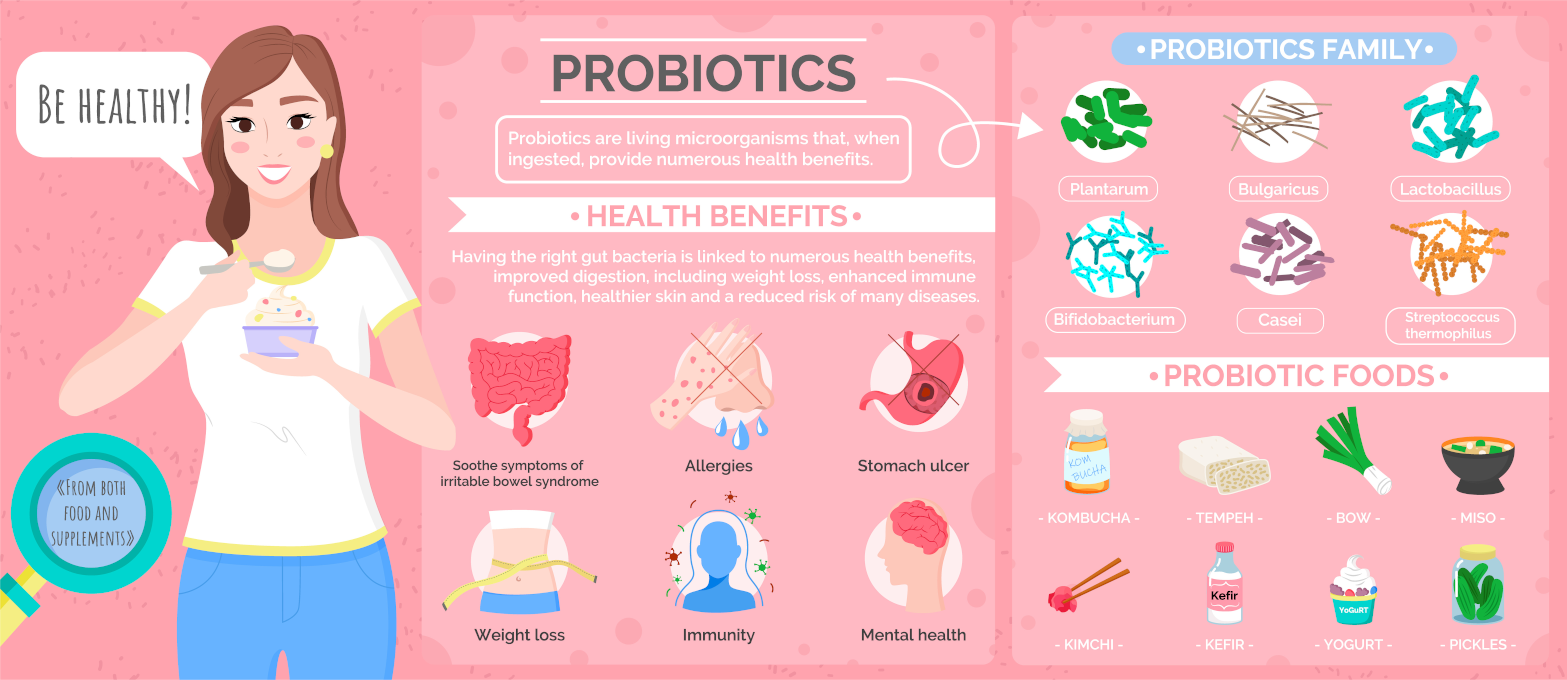
- Probiotics. We need friendly bacteria to repopulate the intestines for their numerous beneficial effects on intestinal health and because they compete with less friendly bacteria that damage the gut wall.
- High-potency vitamin/mineral supplement
- Vitamins C and E are the primary antioxidants.
- Zinc deficiency is a well-known complication in IBD, occurring in 45% of sufferers. Zinc deficiency leads to poor healing of fissures and fistulas, skin lesions, retinol dysfunction, lowered immunity and poor appetite.
- Folic acid deficiency results in abnormalities of the intestinal mucosal cells, promoting malabsorption and diarrhoea.
- Vitamin B12. B12 is absorbed in the part of the intestine most commonly affected in IBD.
- Digestive enzymes can reduce inflammation of Inflammatory bowel disease and help with digestion.